WHAT IS OBSTRUCTIVE SLEEP APNEA
Obstructive sleep apnea is the continuous and repeated pauses in breathing due to obstruction of the upper airways during sleep. These pauses in breathing may be complete (apneas) or partial (hypopneas) and having as a result the disruption of gas exchange and cessation of normal sleep.
Apnea refers to the pause in breathing for ten (10) seconds or more. Hypopnea is defined as reduction in ventilation of at least 50% that results in a decrease in arterial saturation of 4% or more due to partial airway obstruction.
The most benign indication of the increased airway resistance is snoring. According to published statistics, snoring is sporadically observed in approximately 27% of children while the 7-12% of children appear recurrent snoring (that is repeated more frequently than three days a week).
ETIOLOGY AND AGGRAVATING FACTORS
Obstructive sleep apnea is caused by the reduction of the upper airways patency during sleep, thereby making it difficult to airflow despite the existence of respiratory effort. During sleep, it is observed reduction in the diameter of the airways due to reduced tonicity of the pharynx muscles and palate.
Further reduction of the airways patency leading to obstructive apnea that can be caused by:
- Hypertrophy of the tonsils and adenoids (common cause of obstructive apnea)
- Allergic rhinitis
- Inhalation of tobacco smoke in smokers environment
- Neuromuscular disorders or hypotonic situations
Another aggravating factor is childhood obesity which has reached epidemic proportions.
Serious obstructive sleep apnea (which could present an immediate risk to the life of infant or child) may cause anatomical anomalies of craniofacial complex or larynx, such as:
- Micrognathia (small lower jaw) that is observed in syndromes (Treacher Collins, Pierre Robin Sequence)
- Syndromes with premature synostosis of sutures at the skull base and face (Crouzon, Apert, Pfeiffer etc.).
- Laryngomalacia
DIAGNOSIS
The symptoms of obstructive sleep apnea are often perceived by parents (snoring, noisy breathing, restless sleep, retraction of the chest during inspiration (see photo from the Pierre Robin Sequence).
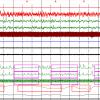
Since the symptoms are not always typical, diagnosis that is based only on medical history taking is not sufficient. It is required a high index of suspicion on the part of the pediatrician, and often the accurate diagnosis requires laboratory confirmation with study and recording of sleep (patterns) in special laboratories. During the study of sleep, many parameters are recorded and evaluated (EEG, Oculogram, hemoglobin saturation measurement, measurement of airflow in the nose, respiratory effort).
THE CONSEQUENCES OF OBSTRUCTIVE SLEEP APNEA
The insufficient normal and refreshing sleep may cause sleepiness during the day, a sense of fatigue and distraction. It is also considered that the obstructive sleep apnea may be involved in cases of hyperactivity as well as other cognitive and learning disorders.
Even slight disturbances in sleep structure may affect metabolic function; it is speculated that it may be affected the release of growth hormone causing developmental delay.
The obstructive sleep apnea may also affect cardiac function and lead to hypertension.
TREATMENT OF OBSTRUCTIVE SLEEP APNEA
In milder cases, where there is no obvious anatomical aggravating factor, except maybe the mild micrognathia (small lower jaw), the situation can be assisted with the construction of a special splint which the child wears during sleep. This splint promotes the lower jaw and tongue, thus freeing the breath.
If it is found tonsillar hypertrophy, then the appropriate first-line therapy is the tonsillectomy and adenoidectomy (adenoids). This surgery usually improves or solves the problem. But, parents must be aware that in approximately 13-29% of cases, obstructive sleep apnea continues to exist after the surgery. If obesity coexists, then the percentage rises up to 73%.
In cases of syndromes with premature synostosis at the base of the skull and face (Crouzon, Apert, etc.) when usually coexists brachycephaly (reduced anteroposterior diameter of the head), the problem is much more serious. The upper airways are extremely "shrunken" and not allow the free flow of air while the brain is depressed due to the reduced capacity of the skull. The only solution is the shifting of the frontal part of the skull and face forward which effectively increases the dimensions of the upper airways and restore breathing. At the same time, the capacity of the skull is increased resulting in decompression of the anterior part of the skull and its better oxygenation. It is about a large surgery with the potential of serious complications which is performed in organized craniofacial centers. The surgery is usually performed at the age of 10-12 years. Up to then, apnea is treated with smaller surgeries such as tonsillectomy and adenoidectomy, cauterization of hypertrophic mucus in nose (lower turbinates) or/and using the CPAP machine.
CPAP MACHINE
The CPAP machine (Continuous Positive Airway Pressure) is a portable respirator used in the treatment of obstructive sleep apnea. It is linked with special mask with the child's face during sleep and slightly increases the pressure of inhaled air in order to overcome the resistance of the airways.
This device is an important aid to the problem of obstructive sleep apnea in appropriate cases, but it is required conformation on the part of the child and its usage is not always tolerable.